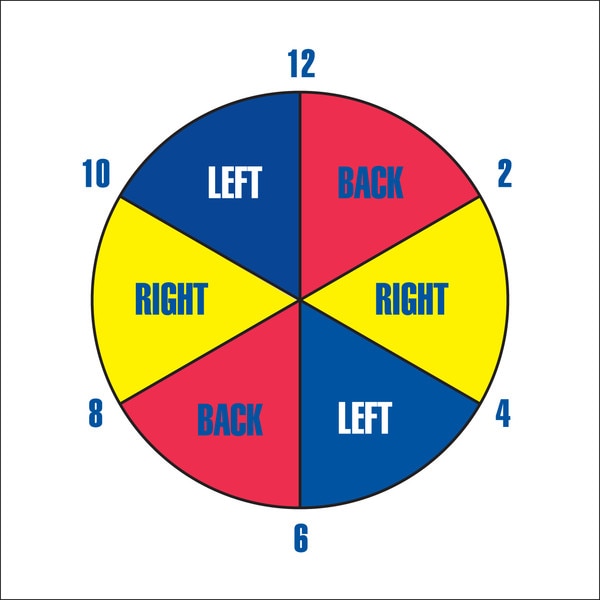
Printable Turning Schedule Clock
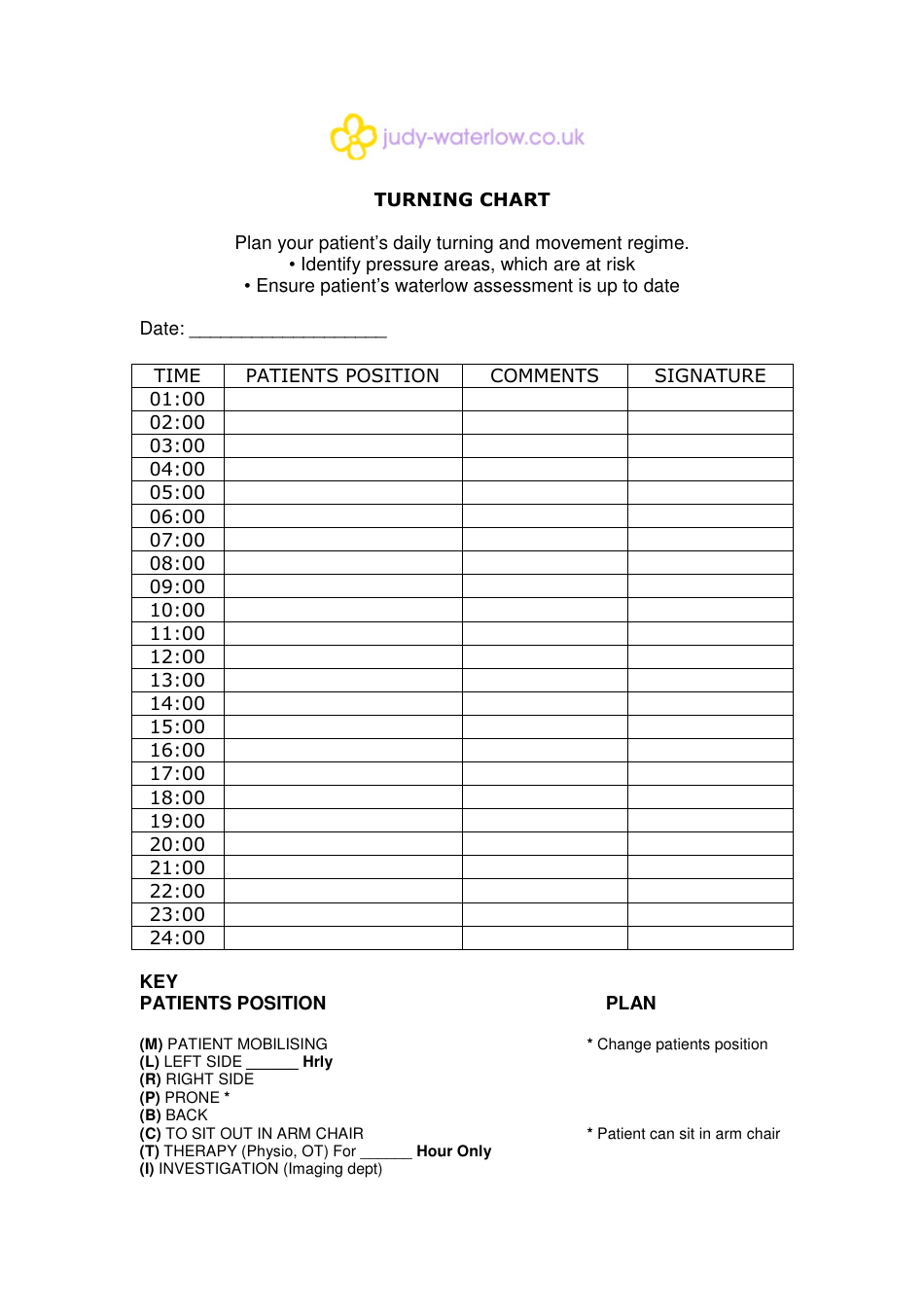
Printable Turning Schedule Clock - This bed turning schedule outlines a patient's positioning every 2 hours over a 12 hour period, alternating between supine lying on their back and left and right side lying positions to prevent. In this paper, we present a scheduling algorithm that uses data from a pressure mat on the hospital bed to compute a repositioning schedule that minimizes nursing staff interaction while. At 0600, the patient is repositioned from their left side onto their back. List components of a best. Implement best practices for safe patient handling and help reduce injury to caregivers and patients. The document provides a turning schedule for 12 hours, listing a direction to turn (left, right, or flat) every two hours, with left, flat, right, and flat turns alternating throughout the day and night. Turning schedule* *supine/back position is intentionally omitted from schedule due to frequent incidental supine positioning throughout the day (e.g. Frequency of positioning, the type of position and time. Turn the patient every two hours to the corresponding position. The turning clock is an interactive communication tool placed at resident’s bedside that outlines the individual positioning plan including; Create this form in 5 minutes!. Discover the turn clock, a helpful tool for repositioning patients to prevent bed sores. Distinguish between an avoidable and an unavoidable pressure ulcer. This document provides a turning schedule for a patient requiring repositioning every 2 hours. Time is expressed in military format. This tells the caregiver what position the patient or resident should be in at that time to promote proper. Simply fill out the form to access your. At 0600, the patient is repositioned from their left side onto their back. In this paper, we present a scheduling algorithm that uses data from a pressure mat on the hospital bed to compute a repositioning schedule that minimizes nursing staff interaction while. Turning schedule* *supine/back position is intentionally omitted from schedule due to frequent incidental supine positioning throughout the day (e.g. Create this form in 5 minutes!. The turning clock is an interactive communication tool placed at resident’s bedside that outlines the individual positioning plan including; Discover the turn clock, a helpful tool for repositioning patients to prevent bed sores. Start with these dos and don’ts. Edit and esign printable turning and repositioning chart to ensure excellent communication throughout the form. In this paper, we present a scheduling algorithm that uses data from a pressure mat on the hospital bed to compute a repositioning schedule that minimizes nursing staff interaction while. Turning schedule* *supine/back position is intentionally omitted from schedule due to frequent incidental supine positioning throughout the day (e.g. Indoff ct is a master at producing quality dry erase boards.. This tells the caregiver what position the patient or resident should be in at that time to promote proper. At 0600, the patient is repositioned from their left side onto their back. Explain three justifications for a pressure ulcer prevention program. Frequency of positioning, the type of position and time. Turning schedule* *supine/back position is intentionally omitted from schedule due. List components of a best. The schedule lists the positions of supine, left side, and right side to be followed from 8 am to 8 am. In this paper, we present a scheduling algorithm that uses data from a pressure mat on the hospital bed to compute a repositioning schedule that minimizes nursing staff interaction while. Frequency of positioning, the. List components of a best. Implement best practices for safe patient handling and help reduce injury to caregivers and patients. This bed turning schedule outlines a patient's positioning every 2 hours over a 12 hour period, alternating between supine lying on their back and left and right side lying positions to prevent. Explain three justifications for a pressure ulcer prevention. This tells the caregiver what position the patient or resident should be in at that time to promote proper. Discover the turn clock, a helpful tool for repositioning patients to prevent bed sores. At 0600, the patient is repositioned from their left side onto their back. List components of a best. The document provides a turning schedule for 12 hours,. Distinguish between an avoidable and an unavoidable pressure ulcer. Explain three justifications for a pressure ulcer prevention program. Create this form in 5 minutes!. Learn how to use this tool effectively for better patient care. Time is expressed in military format. This document provides a turning schedule for a patient requiring repositioning every 2 hours. The schedule lists the positions of supine, left side, and right side to be followed from 8 am to 8 am. In this paper, we present a scheduling algorithm that uses data from a pressure mat on the hospital bed to compute a repositioning schedule that. This bed turning schedule outlines a patient's positioning every 2 hours over a 12 hour period, alternating between supine lying on their back and left and right side lying positions to prevent. Turn the patient every two hours to the corresponding position. This tells the caregiver what position the patient or resident should be in at that time to promote. Simply fill out the form to access your. In this paper, we present a scheduling algorithm that uses data from a pressure mat on the hospital bed to compute a repositioning schedule that minimizes nursing staff interaction while. This tells the caregiver what position the patient or resident should be in at that time to promote proper. Explain three justifications. The schedule lists the positions of supine, left side, and right side to be followed from 8 am to 8 am. Indoff ct is a master at producing quality dry erase boards. The turning clock is an interactive communication tool placed at resident’s bedside that outlines the individual positioning plan including; Implement best practices for safe patient handling and help reduce injury to caregivers and patients. Frequency of positioning, the type of position and time. At 0600, the patient is repositioned from their left side onto their back. Discover the turn clock, a helpful tool for repositioning patients to prevent bed sores. This bed turning schedule outlines a patient's positioning every 2 hours over a 12 hour period, alternating between supine lying on their back and left and right side lying positions to prevent. Simply fill out the form to access your. This document provides a turning schedule for a patient requiring repositioning every 2 hours. This tells the caregiver what position the patient or resident should be in at that time to promote proper. Learn how to use this tool effectively for better patient care. In this paper, we present a scheduling algorithm that uses data from a pressure mat on the hospital bed to compute a repositioning schedule that minimizes nursing staff interaction while. Start with these dos and don’ts. List components of a best. Distinguish between an avoidable and an unavoidable pressure ulcer.Printable Turning Schedule Clock
Printable Turn Schedule Clock
Printable Turning Schedule Clock
Printable Turning Schedule Clock Printable Calendars AT A GLANCE
Printable Turning Schedule Clock For
Printable Turning Schedule Clock
Printable Turning Schedule Clock
Printable Turning Schedule Clock
Printable Turning Schedule Clock
Printable Turning Schedule Clock
Time Is Expressed In Military Format.
Turning Schedule* *Supine/Back Position Is Intentionally Omitted From Schedule Due To Frequent Incidental Supine Positioning Throughout The Day (E.g.
Turn The Patient Every Two Hours To The Corresponding Position.
Create This Form In 5 Minutes!.
Related Post: